This paper is designed to help readers understand the new corona virus and why it has inevitably led to the quarantine measures currently imposed. I will refer to the virus as the COVID-19 virus, as does the W.H.O., instead of using the official, but confusing, name SARS-CoV-2. The official name of the disease is COVID-19.
Historical background
A novel coronavirus, similar to the virus that caused the 2003 SARS (severe acute respiratory syndrome) epidemic appeared in China in December 2019 or earlier. It caused a new syndrome with primarily respiratory symptoms. The degree of rapid spread was phenomenal in the megacity of Wuhan, population 11 million. Wuhan ran out of gear, doctors, hospital beds. The Chinese government was able to commandeer supplies, doctors and nurses from other provinces, and retrain medical professionals to cope with an extraordinarily infectious, and sometimes lethal, virus. This included having doctors put on full PPE--being covered head to toe, and not changing out the gear for a full 12-hour shift. No bathroom breaks, no meals. They have worked 7 days a week, with no time off. Doctors have been housed in hotels and unable to visit family members--not that they wanted to visit, since contact might spread the disease to their families. With extraordinary lockdowns, China gained control of its epidemic. The western press portrayed this as another example of China's authoritarian regime. Little did they know.
The Chinese report that almost all people who catch this disease are symptomatic. But 80-85% have only mild symptoms and can be left to care for themselves at home with rest and fluids. However, about 15% of those diagnosed required hospitalization, due to lack of oxygen from extensive viral pneumonia. One third of these, or 5% of all cases, required ICU care and frequently needed to be placed on mechanical ventilation. Some percentage of total cases, probably about 2-4% in China but about 8-10 % in Italy, which has an older population, could not be saved despite the most aggressive medical measures, and died of this disease. Italy found considerably more of its population required ICU care.
It is possible that many more people than we know have asymptomatic cases, and that our statistics make things look worse than they are. I certainly hope so. But I have seen no evidence to support this hope.
I had assumed the Chinese, who were practiced in handling such diseases after SARS, would get this one under control expeditiously, and much more quickly than has happened.
This assumption turned out to be wrong. Why? It turns out that while this virus's mortality rate is not as high as mortality from SARS (10%) or MERS virus (33% mortality,) it has other features that make it much more contagious. These were not immediately appreciated in China, and it took far too long for this to be appreciated elsewhere in the world.
The Covid-19 virus is extraordinarily contagious
1. The COVID-19 virus led to 1,000 times as much virus (500,000,000 viral particles on a swab) present in the throat as compared to the SARS virus (500,000 particles). While we don't yet know how many viral particles it takes to cause an infection, if there are 1000 times as many particles being expelled with a cough or sneeze, or when simply breathing, breathing indoor air shared with someone who is infected is likely to be a significant risk factor.
2. Unlike most infections, this virus appears to be contagious even before symptoms occur and even after patients appear to have resolved the infection. SARS was contagious only after several days of illness, enabling effective quarantines to be implemented. For this virus, the highest viral titers are measured at the beginning of illness, prior to diagnosis. When the COVID-19 virus is contagious when cases are asymptomatic, there is no way to impose effective quarantines on the infected, without testing everyone.
On average, it takes 5 days from exposure until onset of symptoms, but may take up to 14 days and rarely longer.
Inadequate Testing
Number of specimens tested for SARS-CoV-2 by CDC labs (N=3,995) and U.S. public health laboratories* (N=15,749)†
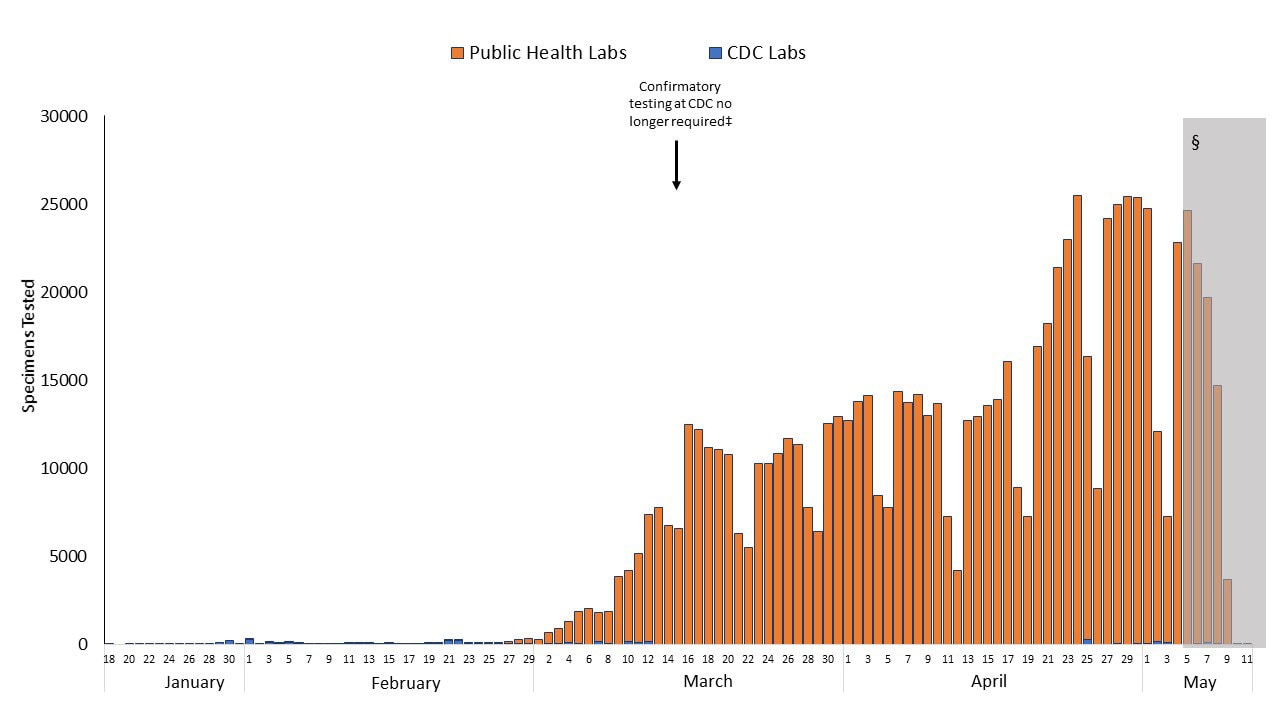
The CDC restricted testing to all but a tiny number of those with compatible symptoms, as CDC acknowledges in its graph, above. Had there been the availability of widespread reverse transcriptase PCR testing, or had other types of tests had been made available, and if the US had been able to test cases with minimal or no symptoms, maybe the US or other nations could have instituted quarantines that stopped spread. But as you know, the CDC made the inexplicable decisions to restrict US testing by allowing only the test CDC had developed to be used, a test that was both unnecessarily cumbersome, and faulty, and to test only those who almost certainly were infected. This slowed down the development of better and more accessible tests by private, university and state public health labs. CDC's ban on other tests was only lifted on February 28. (Tom Frieden, former CDC Director, has called for an independent panel to investigate what went wrong.)
After Feb. 28, FDA offered to approve new COVID virus tests using its authority under an Emergency Use Authorization. But that, too, held up the use of new tests until FDA approved them. Finally, to avoid another bottleneck, this past week FDA said that any entity could start using its own tests, and apply for approval later.
After Feb. 28, FDA offered to approve new COVID virus tests using its authority under an Emergency Use Authorization. But that, too, held up the use of new tests until FDA approved them. Finally, to avoid another bottleneck, this past week FDA said that any entity could start using its own tests, and apply for approval later.
The prolonged duration of infectivity
One study found that the median length of time during which patients were contagious was 20 days. One patient had detectable virus for 37 days. The duration of contagion might even extend further in some cases, because patients who died tended to remain contagious throughout their course. Let me repeat myself: patients were contagious before they showed symptoms, during their symptomatic phase, and even after they recovered. This makes it impossible to identify those who are spreading the disease. It also makes it impossible to keep hospitals (and other indoor spaces) clean.
Airborne vs Droplet spread
When you cough or breathe, particles of air, virus and water are expelled. The old dogma said that most illnesses produce exhaled particles greater than 5 µ in size (droplets), which fall to the ground within 3 feet of the person producing them. Particles smaller than 5 µ in size could travel further, up to 6 feet away from the person who expelled them. However, very small particles could stay suspended in air for hours or days. Newer research tells us that we breathe out particles of many different sizes, and that 3' and 6' distancing does not account for airborne particles. Some of what we exhale falls close to us, while other particles remain suspended in the air for indefinite periods, and can travel on air currents.
Once particles fall out of the air, they usually contain viable virus and contaminate the surfaces onto which they fall. The COVID virus is more dangerous as a large droplet, but can still spread as tiny particles that remain suspended in air for hours and perhaps a few days. Indoor air becomes a risk, especially in closed spaces like elevators, which are used by large numbers of people.
Once particles fall out of the air, they usually contain viable virus and contaminate the surfaces onto which they fall. The COVID virus is more dangerous as a large droplet, but can still spread as tiny particles that remain suspended in air for hours and perhaps a few days. Indoor air becomes a risk, especially in closed spaces like elevators, which are used by large numbers of people.
Negative pressure rooms in hospitals suck indoor air out of infected patients' rooms, preventing virus from contaminating hospital halls and other areas.
CDC describes such rooms here.
The preferred placement for patients who require Airborne Precautions is in an airborne infection isolation room (AIIR). An AIIR is a single-patient room that is equipped with special air handling and ventilation capacity that meet the American Institute of Architects/Facility Guidelines Institute (AIA/FGI) standards for AIIRs (i.e., monitored negative pressure relative to the surrounding area, 12 air exchanges per hour for new construction and renovation and 6 air exchanges per hour for existing facilities, air exhausted directly to the outside or recirculated through HEPA filtration before return).
But there are not enough negative pressure rooms for COVID-10 patients, especially in ICUs and ERs. So you cannot keep the air and surfaces in a hospital entirely free of virus. ICUs with all their equipment will be contaminated. The only thing to do is to have everyone working in the hospital wear full airborne personal protective equipment, from head to toe, all day long. This is what Chinese doctors had to do. But what will happen to the other, non-COVID patients? Some will be exposed. Visitors must be banned. This is probably why hospitals are trying to empty themselves of patients: both for the predicted onslaught of new patients, and to minimize the number of patients who will be exposed to the COVID-19 virus while being treated for something else.
One solution is to create separate hospital facilities for COVID patients and for everybody else. This, of course, requires being able to test and identify those with infection.
Duration of infectivity on surfaces
Bacteria and viruses don't die like people do. People are either alive or dead. But the COVID virus, like other microorganisms, is found in colonies or groups and their number slowly falls over time. The number of viruses in these groups "decay" logarithmically, instead of dying all at once.
Let's say you have 1 million viral particles on a copper surface. Copper, btw, is the surface that destroys virus the fastest. After one half-life, which usually is, say one hour, half will still be viable: 500,000. After another hour, half of those, or 250,000 will remain viable. After 24 hours, you will no longer have viable viral particles. Virus lives longer on glass, plexiglass and steel surfaces. This applies to uncleaned surfaces.
So, if you don't handle contaminated items for several days, probably enough of the virus will have died to make your risk negligible. But if you want to touch something sooner, you will need to decontaminate the surface. Here is a review article with good answers for what works and how long you need to keep your disinfectant in contact with the surface. I summarize:
Bleach (sodium hypochlorite) 0.21% dilution on a surface for one minute. Different bottles of bleach have different concentrations, so calculate your dilution accordingly. One part hypochlorite per thousand parts water. Roughly 1/3-1/2 cup bleach per gallon water.
Hydrogen peroxide 0.5% dilution for one minute
Alcohol 70% or more concentration, for 30 seconds. Lower concentrations may also work but testing was limited.
Be aware that virus lives on cardboard, paper, clothing for days. Washing clothes daily, not wearing outdoor shoes into the house, and frequent showering will all reduce the amount of virus you harbor.
Personal protective equipment (PPE) for healthcare workers
What is full airborne personal protective equipment? This is what healthcare workers used for the Ebola epidemic. We use a little less gear for active tuberculosis. It means being covered head to toe with disposable suits, caps, gloves, shoe covers, nose/mouth and eye coverage, and often a clear visor in front of the face.
I have rarely had to use eye protection with patients before, nor was it considered necessary to use a plexiglass face shield. But the diseases hospital doctors were previously exposed to (apart from Ebola) were treatable, and we almost never got them, and virtually never died from them if we did. This disease is different.
An estimated 1,700 healthcare workers (HCWs) in Italy have become infected, 8% of the total number of cases. Italy identified its first case only 28 days ago. A number of healthcare workers in China, and now in Italy, have died from the disease. Many HCWs in the US are also infected, some whose condition is critical. PPE are already in short supply.
"Many doctors have been expressly told by their administration not to speak publicly about conditions" in their establishment.
"Many doctors have been expressly told by their administration not to speak publicly about conditions" in their establishment.
Additional tests needed
Ideally we will get accurate (CDC refuses to say how accurate current tests are) and rapid tests for COVID-19 virus, and will be able to put the COVID patients in a separate facility from the other patients when they first present for medical care. We will presumably also get serologic (antibody) tests that will allow us to diagnose immunity. Hopefully this disease confers immunity once you have it, but I have not seen anything published on this yet. No serology tests are available today, although there are reports that they have been developed in other countries, and are surely in development here.
The symptoms of Covid-19
The most common early symptoms of this infection, in roughly descending order, are fever, fatigue, dry cough, headaches, loss of appetite, shortness of breath, muscle pain, occasional sputum production. There is usually no runny nose, diarrhea, or vomiting, but they occasionally occur.
The symptoms of Covid-19
The most common early symptoms of this infection, in roughly descending order, are fever, fatigue, dry cough, headaches, loss of appetite, shortness of breath, muscle pain, occasional sputum production. There is usually no runny nose, diarrhea, or vomiting, but they occasionally occur.
The severe syndrome (based partly on unpublished emails from doctors in the field)
A normal respiratory virus may temporarily fill your lungs with inflammatory materials, but most people, even with severe disease, can be kept alive for a week or two and their body will fight off the infection. As long as you keep them oxygenated they recover. Of course, those with severe underlying conditions may succumb to a final hit by the virus.
This viral disease is different.
1. It lasts longer: people with severe disease tend to spend 2-6 weeks in the hospital, much longer than normal. That means they take up many more hospital beds, and contaminate hospitals longer.
2. It causes a relatively mild viral illness, which usually includes a viral pneumonia, for about a week, then patients may suddenly "crash" with respiratory failure. Acute Respiratory Distress Syndrome (ARDS), which has a mortality around 30-40%, is a common complication. Cytokine storm is another COVID-19 complication, which has a high mortality rate, and may be part of the ARDS syndrome. Those who survive may have significant scarring of their lungs and face a prolonged recuperation.
3. It can affect multiple organs. Some patients have died of cardiac failure (myocarditis) after seeming to start recovering from the viral pneumonia. Virus has been found in heart muscle, gut and liver. It has been isolated from urine and stool, although a minority of patients develop nausea, vomiting or diarrhea. Some patients develop shock and/or multiorgan failure.
While a higher percentage of the elderly and infirm are dying from COVID-19, there are plenty of fit young people being stricken with severe illness or death. Holland says half its COVID-19 ICU patients are under the age of 50. Doctors have no idea why some healthy people develop severe disease and others don't. Probably this is due to genetic differences that have yet to be identified. No adult is in a completely safe demographic. According to CDC, twenty percent of US deaths from the COVID virus have occurred in those aged 20-64. There have been 185 US deaths so far, according to this tracker.
Treatment
Basically, severely ill patients are being supported by iv fluids, oxygen, ventilators, ECMO (extracorporeal membrane oxygenation or artificial lung) machines, but there has been no effective antiviral treatment at the late stages, perhaps because significant scarring has already occurred. And I anticipate we will soon run out of ventilators and ECMO machines.
It is possible that drugs, particularly chloroquine, the related drug hydroxychloroquine, or remdesivir will save the day. I certainly hope so. But I suspect they will need to be used early, before too much damage has already been done. Bayer has offered to donate 3 million chloroquine tablets to the cause. Efforts were announced March 20 by several additional manufacturers to make more chloroquine drugs and donate millions of tablets. (The tablets are OTC and cost about $0.04 each in some countries with malaria.)
Hydroxychloroquine was used on someone I know, early in the COVID-19 course, and seemed to lead to improvement. It is said to be easy to synthesize. And today President Trump started talking about it, calling it a game-changer. I hope he is using his new, wartime powers to ensure the US' ability to produce this drug in huge quantities, immediately.
Hydroxychloroquine was used on someone I know, early in the COVID-19 course, and seemed to lead to improvement. It is said to be easy to synthesize. And today President Trump started talking about it, calling it a game-changer. I hope he is using his new, wartime powers to ensure the US' ability to produce this drug in huge quantities, immediately.
Chloroquine is an antimalarial that was first synthesized 80 years ago. I used it to ward off malaria many years ago, and it is still used in areas where malaria parasites have not developed resistance. It is generally quite safe, though doctors must check patients for drug interactions. Hydroxychloroquine is mostly used in the US for the autoimmune diseases lupus and rheumatoid arthritis. It may also be used in combination with a macrolide antibiotic for Lyme disease, and was used this way in some French COVID-19 patients with reported excellent results. I have used it in dozens of patients safely.
While Dr. Fauci says we need clinical trials to see if chloroquine works against the COVID-19 virus, there are a reported 10 ongoing clinical trials in China looking at the efficacy of this drug. (Luckily, we don't require safety trials because it is an approved drug with a known safety profile.) There has been a successful small trial of 30 patients in the west. We have ignored the lessons from China at our peril. We need better international collaboration, rather than trying to reinvent the wheel, as CDC attempted to do with testing, and failed. The Chinese are a very smart people, and they are practical. What have they learned so far?
While Dr. Fauci says we need clinical trials to see if chloroquine works against the COVID-19 virus, there are a reported 10 ongoing clinical trials in China looking at the efficacy of this drug. (Luckily, we don't require safety trials because it is an approved drug with a known safety profile.) There has been a successful small trial of 30 patients in the west. We have ignored the lessons from China at our peril. We need better international collaboration, rather than trying to reinvent the wheel, as CDC attempted to do with testing, and failed. The Chinese are a very smart people, and they are practical. What have they learned so far?
Why all the fuss? Why is everything being shut down?
Here's the problem: the exponential increase in cases of a severe disease is unprecedented. Because of its unique, extremely high degree of infectiousness, plus stability in the environment, lots of people will be exposed to this disease at the same time. About five days later they will get sick. About ten days later they will be filling up hospitals. And a week or two after that, people will start dying. Hospital visits, admissions and deaths will skyrocket at exponential rates. On March 20, Italy has lost over 600 people to the COVID-19 virus during the past 24 hours, and over 4,000 so far.
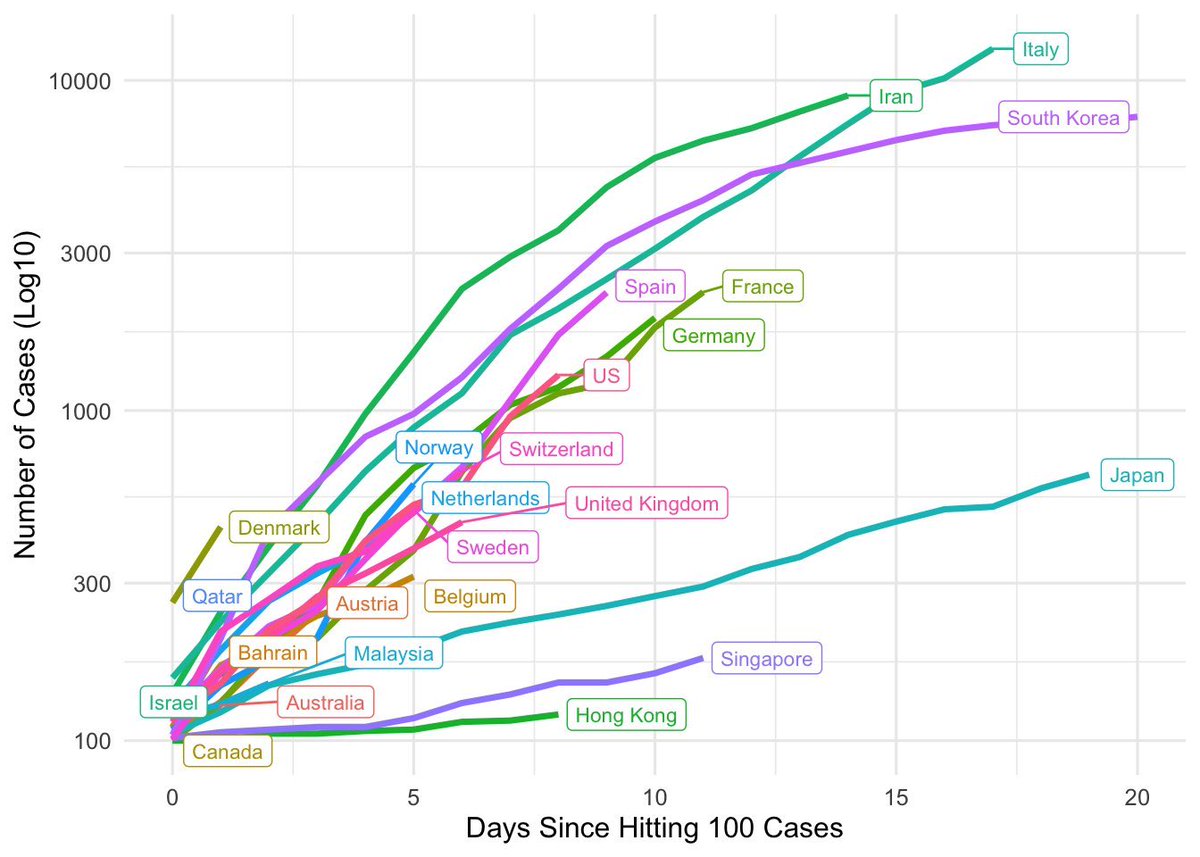
As shown in a graph below by Eric Feigl-Ding: (note Y axis scale is logarithmic)
Europe and US are mostly all on the same path. Note log Y-axis (linear=exponential; steeper line is more exponential, faster spread). Japan also has limited testing. Only South Korea, Singapore and Hong Kong have it under control or improving. #COVID19
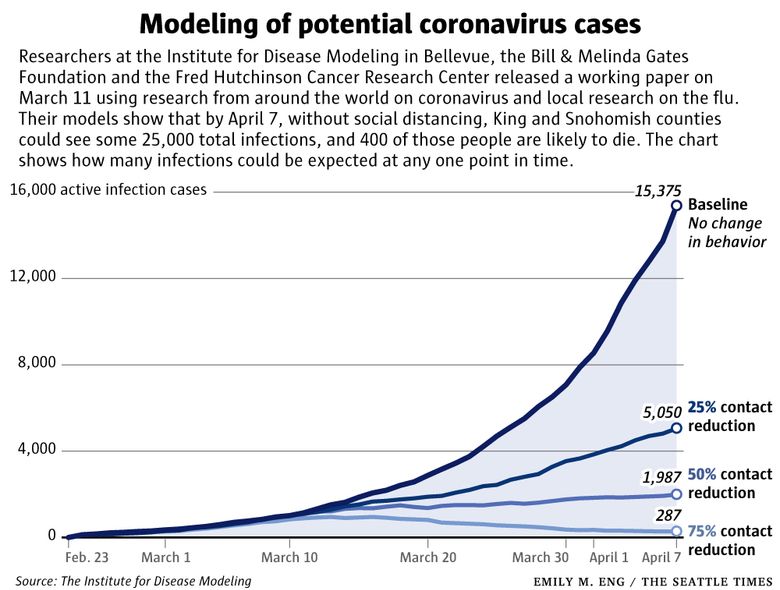
But if you reduce contact with other people, you can make a huge impact on cases:
Here's the doomsday scenario: doctors and nurses may refuse to go to work, because they themselves cannot be protected due to the lack of protective equipment. Even if all our healthcare workers keep working (and Italy just graduated its doctors 9 months early to provide extra manpower, and asked recently retired doctors to come back to work) there will still not be enough hospital beds, ICUs and ventilators to treat the massive influx of patients who are expected to arrive en masse. Many people will be refused care. Many people will die at home, or on the streets.
This is a scenario that is unacceptable to politicians, for they initially responded poorly to this crisis, and know they will never be re-elected unless they do something effective, and fast.
The period during which testing and isolation of cases would have halted spread is over. That window was missed. That opportunity is gone.
In order to avoid a catastrophic crash of the healthcare system, the only solution is to stop people from giving this virus to each other, right now. We can't all be sick around the same time, or there will be pandemonium. Probably millions of Americans are already infected. Why do I say this? The governor of Ohio and Ohio's chief health officer said, one week ago, that they already knew at least 1% of Ohioans were infected. I assume they have access to more accurate data than the public on this.
So, a total shutdown and isolation is needed, because there is no other way for the health system to bear the number of cases that are expected. College dormitories will be converted into Covid-19 hospitals. Military hospital ships will be sent to areas of greatest need. Supplies from the defense department and the CDC's Strategic National Stockpile will be shared with civilian healthcare entities. But these supplies will be nowhere near enough. Unless we massively reduce transmission right now, we will face a dire situation very soon.
The term "flattening the curve" means slowing down spread of virus, even though (presumably) the same number of people will be infected by the end of the epidemic. It means that the epidemic will be slowed, and last longer, but large numbers of unnecessary deaths caused by a crash of the healthcare system will be avoided. And that is huge. It also buys time to manufacture the masks, ventilators, and drugs that will be needed. It buys time to find new drugs that may be effective.
Isolation from everyone but the people you live with is critical. Please take this situation seriously, and do your best to comply. Here are my recommendations, posted last week, on how best to avoid infection.


















2 comments:
Thank you Meryl,
Your thoughts and analysis is in depth. Your keeping things in layman terms for us assists in my understanding.
Steve F
Thank you Meryl Nass. The clearest and most helpful analysis I have read to date. Best to you always,- Roc
Post a Comment